Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the only known curative therapy for myelodysplastic syndromes (MDS). The decision of allo-HSCT depends on prognostic scoring models such as revised international prognostic scoring system (IPSS-R) which include cytogenetic abnormalities, cytopenia, and % of bone marrow (BM) blasts. Recently, the prognostic role of genomic profile in MDS patients is arising. However, it is hard to conduct the next generation sequencing to all MDS patients in the real-world. Therefore, we aimed to evaluate the prognostic impact of BM cellularity at diagnosis as a new clinical prognostic factor of MDS with allo-HSCT.
A total of 122 patients with MDS patients who underwent allo-HSCT between July 2009 to August 2022 in single center were analyzed retrospectively. Overall survival (OS) was analyzed using the Kaplan-Meier survival curves according to the BM cellularity at diagnosis. The potential prognostic parameters were evaluated for OS by uni-and multivariate cox-regression analysis.
All patients were eligible for allo-HSCT and median age of 61.5 years (range: 19-71). Median follow-up duration was 36.9 (IQR 17.6-72.4) months. The 3-year and 5-year OS were 60.1% (95% CI 51.6-69.0) and 52.5% (95% CI 42.8-61.3), respectively. IPSS-R risk group was classified as very low (6, 4.9%), low (15, 12.2%), intermediate (40, 32.8%), high (37, 30.3%) and very high (24, 19.7%). Seventeen patients (13.9%) had complex karyotype at diagnosis. Seventy-seven patients (63.1%) were treated with hypomethylating agents before allo-HSCT. Most patients (70, 57.4%) had less than 5% BM blasts at allo-HSCT. The majority (74, 60.7%) received reduced intensity conditioning.
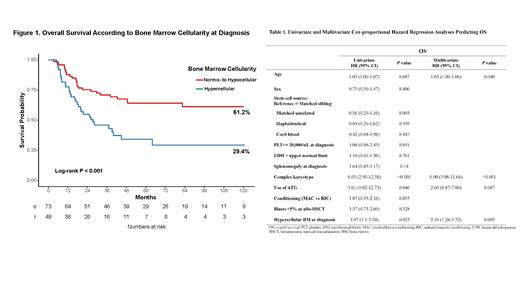
OS significantly differed between patients with hypercellular BM and normo- to hypocellular BM at diagnosis by the log-rank test ( P <0.001) (Figure 1). In multivariate analysis for OS, complex karyotype at diagnosis ( P<0.001; HR 6.00; 95% CI 3.08-11.66), age ( P=0.04; HR 1.03; 95% CI 1.00-1.06) and hypercellular BM at diagnosis ( P=0.005; HR 2.16; 95% CI 1.26-3.72) were associated with worse outcome (Table 1).
In this study, we demonstrated the BM hypercellularity at diagnosis independently predicts the inferior outcome of MDS patients with allo-HSCT. Although further validation with a larger cohort would be needed, it could be helpful to decide the treatment strategy of transplantation eligible MDS patients.
Disclosures
No relevant conflicts of interest to declare.